Items filtered by date: April 2025
When a Total Contact Cast Is Needed

For people battling diabetic foot ulcers, a total contact cast can be a game-changer in the healing process. These casts, meticulously crafted to fit snugly around the foot and lower leg, help to distribute weight evenly across the sole, allowing for effective ulcer management and healing. Diabetes often leads to foot problems, like neuropathy, where individuals lose sensation in their feet. This lack of feeling makes it challenging to detect blisters, cuts, or sores, which can quickly escalate into ulcers if left untreated. Total contact casts are primarily recommended for individuals with diabetic foot ulcers that resist conventional treatment methods. A total contact cast provides a protective shield for the ulcer, allowing it to heal efficiently. By reducing pressure on the affected area, these casts promote faster recovery. Typically, most ulcers show significant improvement within six to eight weeks with the consistent use of total contact casts. While wearing a total contact cast, it is important to prioritize its care and adhere to certain precautions, such as keeping it dry, minimizing walking, watching for complications, and managing itching and discomfort. To find out if a total contact cast is an option for treating your diabetic foot ulcer, it is suggested that you schedule an appointment with a podiatrist for an evaluation.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Geriatrics and Podiatry
Bone density loss, dry skin, poor circulation, and rough and brittle nails are some of the common problems that can occur as people age. The effect that these problems has on foot health should be of particular concern in comprehensive geriatric care.
Feet that are diseased or injured have a negative effect on overall health and safety. Painful feet limit a person’s willingness and ability to stay active. Poor foot health can also cause gait change, which can lead to falls and accidents. Even though recovery time from health problems naturally slows as we age, many foot problems can be avoided altogether with regular prophylactic care.
Feet should be thoroughly washed in warm water daily. Care must be taken to dry the feet well, making sure to dry between and under the toes. Any left-over moisture can cause problems like foot fungus. After cleaning feet carefully check for problems such as cracked skin, bruises, swelling, cuts, corns, or other irregularities.
Examine toenails for ingrown, jagged, or split nails. Long toenails should be cut straight across. Never cut toenails at an angle or down the side as this may lead to ingrown nails.
Cracked and dry feet should be treated once or twice a day with a non-greasy moisturizer. Rub the moisturizer into the skin and allow it to dry before putting on socks and shoes. Sweaty feet can be dusted with a small amount of talcum powder. Avoid putting talcum directly into shoes as this may make feet slip within the shoe and cause a serious fall.
Wear clean dry socks each day. Not only do clean socks feel better on the feet, but socks worn for longer periods may harbor disease and odor-causing bacteria. Socks should not be tight around the top as they can leave marks on the leg. Socks that are too small can bring about bruising caused by pressure against the toes.
Wear comfortable and well-fitting shoes. If possible, consult a professional footwear specialist when purchasing shoes. Do not walk around barefoot as this exposes the feet to possible injury and bacteria.
Good foot health allows a more active lifestyle, which improves blood flow. Good circulation aids in recovery from injury or illness. It is also important for maintaining overall health.
Serious health problems can manifest themselves as symptoms in the feet. The elderly should seek professional help from a podiatrist if experiencing foot problems like tingling, numbness, pain, infection, or a sore that does not heal. Taking care of these problems right away can prevent the development of severe cases.
The Importance of Healthy Blood Flow for Older Feet
 Ensuring good circulation and blood flow in older feet is important for maintaining overall foot health and preventing potential complications. As people age, blood vessels can naturally narrow, reducing blood circulation to the feet. Lower blood flow can contribute to slow wound healing, increased susceptibility to infections, and a higher risk for foot-related problems. Tissues need oxygen and nutrients, which are delivered by the blood. Lifestyle adjustments, such as regular exercise, staying hydrated, and avoiding prolonged periods of sitting, can significantly contribute to better blood flow. Good foot care also involves wearing well-fitting shoes that won’t cut off blood flow. You can take proactive steps towards maintaining foot health by focusing on increasing circulation to the feet, which will reduce the risk of foot problems and help you enjoy an active and comfortable lifestyle. If you have poor blood flow to the feet, it is suggested that you visit a podiatrist who can create a personalized treatment plan and diagnose any other foot-related problems.
Ensuring good circulation and blood flow in older feet is important for maintaining overall foot health and preventing potential complications. As people age, blood vessels can naturally narrow, reducing blood circulation to the feet. Lower blood flow can contribute to slow wound healing, increased susceptibility to infections, and a higher risk for foot-related problems. Tissues need oxygen and nutrients, which are delivered by the blood. Lifestyle adjustments, such as regular exercise, staying hydrated, and avoiding prolonged periods of sitting, can significantly contribute to better blood flow. Good foot care also involves wearing well-fitting shoes that won’t cut off blood flow. You can take proactive steps towards maintaining foot health by focusing on increasing circulation to the feet, which will reduce the risk of foot problems and help you enjoy an active and comfortable lifestyle. If you have poor blood flow to the feet, it is suggested that you visit a podiatrist who can create a personalized treatment plan and diagnose any other foot-related problems.
If you need your feet checked, contact one of our podiatrists of Podiatry Associates of Texas. Our doctors will attend to all of your foot and ankle needs and provide you with quality treatment.
Geriatrics and Podiatry
When people age, some common issues that may occur are bone density loss, dry skin, poor circulation, and rough brittle nails. These issues may also affect your foot health if the necessary steps are not taken to alleviate the problems.
It is important to take care of your feet because feet that are injured or diseased can affect your overall health. Having painful feet hinders your ability to do daily activities or may decrease your willingness to do the things that you need to do.
Visiting Your Geriatrician
As we age, health problems become more likely, so it is essential to visit your doctor for check-ups to ensure that you are doing the best you can to take care of your health. It is recommended to check your feet frequently for any possible cuts, bruises, swelling, corns or any other irregularities.
Taking Care of Elderly Feet
Cracked or dry feet can be treated by applying moisturizer often. It is also important not to wear old socks because the older the sock is, the higher the possibility there will be that there is bacteria there. Wear fresh socks and make sure they fit properly.
Proper foot health means that you can have a more active lifestyle and you will not be bogged down by pain. Foot health also leads to good circulation, which is paramount for overall health.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Essential Insights Into Morton's Neuroma
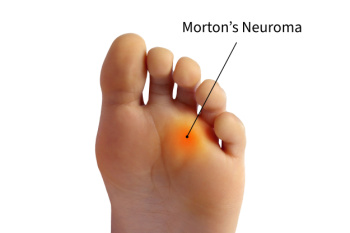
Morton's neuroma, a nerve disorder affecting the feet, is a condition that demands attention and understanding. This ailment is characterized by the thickening of tissues around the nerves that lead to the toes, and it often occurs between the third and fourth toes. Contrary to common belief, it is not a true neuroma, but rather a perineural fibrosis. The primary cause is the compression and irritation of the nerve, resulting in pain, tingling, and a sensation of a lump or pebble in the shoe. High-heeled shoes and tight footwear are frequently implicated in triggering or exacerbating Morton's neuroma. Understanding the symptoms, such as sharp, burning pain in the ball of the foot, is vital for early identification. Proper footwear, foot pads, and orthotics can offer relief, while severe cases may require medical intervention. By grasping the essential facts surrounding Morton's neuroma, individuals can take informed steps towards managing this foot condition. If you have pain between your toes or on the ball of your foot, it is suggested that you consult a podiatrist for a diagnosis and correct treatment methods.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Podiatry Associates of Texas. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Reminder: When Was the Last Time...?
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Monitoring Heel Pain

Monitoring heel pain is essential for effectively addressing its underlying causes and ensuring proper management. Heel pain can stem from various sources, including conditions like plantar fasciitis, Achilles tendonitis, heel spurs, or stress fractures. To gauge heel pain, individuals should focus on several key aspects. First, pinpoint the exact location of the pain, as it can provide valuable insights into its origin. Additionally, identifying activities or movements that trigger or worsen the pain is important. When assessing the severity and duration of the pain, it is also important to assess persistent or escalating discomfort. Signs of swelling, redness, or warmth surrounding the heel area can indicate inflammation. Changes in mobility and any adverse effects on daily activities should be noted. Evaluating footwear choices for proper support and fit can also contribute to managing heel pain. In cases of persistent or severe heel pain, it is suggested that you seek professional evaluation from a podiatrist. Regular monitoring of heel pain allows for early intervention, leading to faster recovery and improved overall foot health.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Three Grades of Ankle Sprains
An ankle sprain occurs when one or more ankle ligament gets overly stretched. Ligaments are strong bands of tissue that bind and support the bones and other structures that make up the ankle. In more severe ankle sprains, the ligament(s) tear—either partially or completely—and there may be an audible popping noise at the moment of injury.
Ankle sprains are quite common and can occur when the ankle rolls outwardly (eversion) or inwardly (inversion), causing the ligament(s) to stretch beyond normal limits, or even tear. Falls, twists, or blows to the ankle during sports or other activities can cause this injury, as well as wearing improper footwear, running on uneven surfaces, or having weak ankles.
Depending on the injury’s severity, an ankle sprain will be classified as Grade I, Grade II, or Grade III. Grade I sprains involve ligament(s) being overly stretched but not torn, with symptoms of mild pain, swelling, and ankle instability. There may also be some difficulty bearing weight. A Grade II sprain usually involves a partial tear of the ligament which brings more intensity in these symptoms, along with possible bruising. With a Grade III sprain, the ligament is completely torn, the symptoms are severe, and it may not be possible to put weight on the affected foot at all.
To diagnose and grade an ankle sprain, a podiatrist will perform a physical examination, checking for tenderness and range of motion in the ankle. For more severe sprains, X-rays or other imaging studies may be necessary.
It is vitally important to have an ankle sprain treated properly as improper healing often leads to future ankle sprains and possibly even chronic ankle stability. Treatment for an ankle sprain will vary, depending on its severity, and may include the RICE method (Rest/Ice/Compression/Elevation), physical therapy, bracing, medications, and possibly even surgery to repair a torn ligament. Rehabilitation is very important for the sprain to heal properly and to restore functionality.
Definition and Causes of an Acute Ankle Sprain

An acute ankle sprain refers to a sudden and unexpected injury to the ligaments that support the ankle joint. These ligaments can become stretched or torn when the foot twists or turns beyond its normal range of motion. This injury often results from a misstep, an awkward landing, or a sudden change in direction, such as in sports activities. The causes of an acute ankle sprain are typically linked to excessive or forceful movements that strain the ankle ligaments. Common situations include stumbling on uneven ground, stepping off of a curb, or rolling the ankle during sports activities, such as basketball or soccer. Wearing high heels and poorly fitting footwear can also increase the risk of ankle sprains by destabilizing the ankle. Understanding the definition and causes of an acute ankle sprain is essential for both prevention and timely treatment. If you have sprained your ankle, it is strongly suggested that you consult a podiatrist who can accurately diagnose this condition, and offer treatment methods that are right for you.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.

