Items filtered by date: December 2019
What Is Morton’s Neuroma?
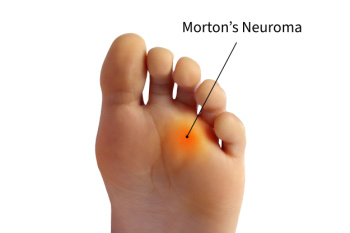
Morton’s neuroma is a painful condition caused by a thickening of tissue around a nerve between the toes, most commonly between the third and fourth toes. It often affects people who wear tight or high-heeled shoes, perform repetitive foot movements, or have foot issues like flat feet or bunions. Symptoms include a burning or sharp pain in the ball of the foot, tingling, or a sensation like there is a pebble in your shoe. The discomfort typically worsens with activity or pressure on the area. Relief options include wearing wider shoes, using cushioned insoles or pads, and taking anti-inflammatory medications. If you have severe pain from Morton’s neuroma, it is suggested that you see a podiatrist who may recommend corticosteroid injections, targeted exercises, or possibly surgery.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Podiatry Associates of Texas. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Arthritis Can Cause Pain in the Feet and Ankles
Differences between Walking and Running Shoes
Both running and walking are great exercises, but should a person wear the same shoes for both activities? The answer is no, because there is a difference between the way a person’s feet hit the ground when they are walking and when they are running. Therefore, the shoes for each activity are designed differently. Before you begin any exercise program it is always recommended that you speak with your doctor or podiatrist.
Walking is a low impact exercise that is often recommended by doctors to their patients. While walking is a simple activity, it still requires some degree of preparation. If you think about walking and how your feet strike the ground as you move, you will notice that your heel hits the ground first before your foot continues to roll forward and your next step begins. Because of this rolling motion, walking shoes are designed to be more flexible than running shoes. This flexibility helps the walker push off with each step taken.
Because the heel hits the ground first when you walk, walking shoes are designed to absorb most of the shock. Walking shoes should therefore have a beveled or angled heel. The angle of the heel helps absorb the shock and reduces pressure from the ankles. This is especially important for speed walkers, as their feet will hit the ground twice as often as the normal walker.
When people decide to run as a hobby or for their health, they must first realize that running is a high impact exercise. If not done with the proper equipment, running may cause damage to the feet and legs. Running shoes are designed to be more lightweight and to have thicker soles. The thicker soles act as shock absorbers for the rest of the body. Walking shoes often do not have the proper arch support that running shoes do.
A proper fitting shoe can make or break a runner or a walker. If the shoes are too big, their feet will slide back and forth inside the shoe and cause blisters. Whether you will be running or walking, the right equipment can make all of the difference in the world.
Walking and Running Shoes and Their Impact on the Feet

Walking and running shoes are designed to meet the specific demands placed on the feet during each activity. Walking shoes typically have a more flexible sole to accommodate the natural rolling motion of the foot as it strikes the ground. They offer cushioning in the heel and arch to provide comfort during prolonged periods of walking. In contrast, running shoes are built to handle the higher impact and repetitive force that running creates. They feature more advanced cushioning, especially in the heel and forefoot, to absorb shock and reduce strain on the joints. Running shoes also offer more support in the midsole to help stabilize the foot during high-impact activities. While walking shoes focus on comfort and support for slower, low-impact movements, running shoes are engineered to provide durability and protection for the faster, more intense demands of running. If you have sustained a foot injury from wearing the wrong shoes for your desired sport, it is suggested that you visit a podiatrist who can treat various foot conditions, and educate you on appropriate shoes to wear.
For more information about walking shoes versus running shoes, consult with one of our podiatrists from Podiatry Associates of Texas. Our doctors can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
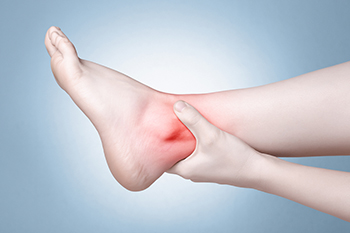
Various Causes of Ankle Pain
Ankles are joints that connect bones in the feet with bones in the lower leg. They are comprised of bones, ligaments, muscles, tendons, blood vessels, and nerves. The ankle joint allows the foot to move side-to-side, as well as up-and-down.
Ankle pain can be caused by a variety of conditions, but is most commonly due to soft tissue injuries such as ankle sprains and strains.
An ankle sprain occurs when one or more of the strong ligaments that support and stabilize the ankle become overly stretched or even torn if the ankle rolls, turns, or twists awkwardly. Depending on the grade of sprain (mild-moderate-severe), there will be varying degrees of pain, swelling, and restricted range of motion, along with tenderness, bruising, and ankle instability. There may even be an audible popping noise at the moment of injury.
Ankle strains can sometimes produce similar symptoms of pain, swelling, and loss of motion, however, they are due to overly stretched muscles and tendons—not ligaments. Ankle strains may also cause muscle cramps in the feet, calves and shins.
Ankle fractures are another common source of ankle pain and occur one or more of the three bones in the ankle become fractured (broken). These breaks can be stress fractures (due to repetitive stress) or traumatic fractures (due to an acute injury). Depending on where and how severe the fracture is, symptoms can include pain and swelling that can sometimes spread up to the knee, bruising or discoloration, and an inability to bear weight. A visible deformity or exposed bone may occur in severe fractures.
Various forms of arthritis may also cause ankle pain. Rheumatoid arthritis (RA) causes the immune system to attack healthy joints, like the ankle joint, by mistake, causing stiffness and swelling in both ankles. Osteoarthritis occurs when cartilage covering the ends of bones wears down, causing the bones to rub against each other. This results in pain, stiffness, and reduced range of motion in the ankle. Gout is a form of arthritis where excess amounts of uric acid in the bloodstream crystallize and build up on joints, causing severe pain and swelling. Reactive arthritis causes joint pain and swelling in the ankle in response to an infection in another part of the body.
Other forms of ankle pain include bursitis (an inflammation of a cushioning bursa sac between tendons and bone), scleroderma (a thickening of connective tissues), chronic ankle instability (caused by improperly healed ankle sprains), Achilles tendon injuries, flat feet, or an infection in the ankle.
What Can Cause an Ankle Rash?
Ankle rashes can occur due to a variety of factors, and identifying the cause is key to effective treatment. One common cause is contact dermatitis, which happens when the skin reacts to an irritant or allergen. This could include new soaps, lotions, or even certain fabrics. Allergies to foods, medications, or insect bites can also trigger rashes on the ankles, often accompanied by itching and redness. Hives, which are raised, red welts that appear suddenly, can develop in response to stress, certain foods, or medications. Another cause of ankle rashes is sunburn, which can occur when the skin is overexposed to UV rays, leading to redness, pain, and peeling. In some cases, fungal infections like athlete’s foot can cause a rash on the ankles. If an ankle rash persists or worsens, it is suggested that you consult a podiatrist who can determine the underlying cause, and guide you toward appropriate treatment methods.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with one of our podiatrists from Podiatry Associates of Texas. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
How Vitamin Deficiencies Can Lead to Cracked Heels

Cracked heels can be uncomfortable and unsightly, and vitamin deficiencies may contribute to their development. Insufficient levels of certain vitamins, especially from the B-vitamin group, can cause the skin to become dry and brittle, leading to cracks. Vitamin B1, also known as thiamine, plays a key role in maintaining healthy skin, and a deficiency can result in rough, cracked skin on the feet. Vitamin B3, or niacin, helps the skin retain moisture and improve its elasticity, preventing cracks. Vitamin B6 supports the body's ability to repair damaged tissues, including the skin, while vitamin B12 is vital for maintaining skin health and preventing dryness. A lack of these vitamins can impair the skin’s ability to stay hydrated and repair itself, making the heels more prone to cracking. If you have developed cracked heels, it is suggested that you contact a podiatrist who can effectively treat this condition.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Dealing With Toenail Fungus

Toenail fungus, or onychomycosis, is caused by fungi that invade the nail bed, leading to discoloration, thickening, and even crumbling of the nail. Factors contributing to this infection include warm, moist environments, improper foot hygiene, and underlying health issues like diabetes or a weakened immune system. Symptoms often include yellow or brown discoloration, a foul odor, and discomfort in severe cases. Treatment options range from topical antifungal medications to oral prescriptions and, in persistent cases, laser therapy or nail removal. A podiatrist specializes in foot health and can accurately diagnose toenail fungus, recommend effective treatments, and provide advice on preventing future infections. If you suspect you have toenail fungus, consider scheduling an appointment with a podiatrist. Early intervention can help restore your nail health and prevent complications, allowing you to enjoy healthy, beautiful feet again.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our podiatrists of Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.

