Items filtered by date: December 2019
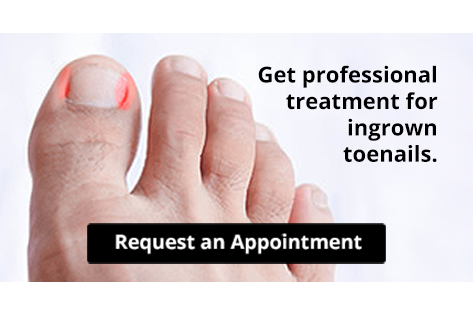
Are You Suffering From Ingrown Toenails?
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
Athlete’s Foot Relief and Prevention
 Athlete's foot is a common fungal infection affecting the skin on the feet, especially between the toes. It occurs due to the growth of dermatophytes, a type of fungus that thrives in warm, moist environments like locker rooms, showers, and even sweaty shoes. Symptoms include itching, burning, and stinging sensations, in addition to red, scaly, and cracked skin. Sometimes, it can also cause blisters or ulcers. Athletes and individuals who frequently wear tight-fitting shoes or who have sweaty feet are at higher risk. Diagnosis is typically made through a physical examination, and sometimes a skin scraping to confirm the presence of the fungus. Possible relief can include antifungal creams, powders, or sprays, and in more severe cases, oral medications. To prevent athlete’s foot, keep feet clean and dry, change socks regularly, wear breathable footwear, and avoid walking barefoot in communal areas. If you have athlete’s foot with persistent or severe symptoms, it is suggested that you visit a podiatrist for advanced treatment which often includes prescribed medication.
Athlete's foot is a common fungal infection affecting the skin on the feet, especially between the toes. It occurs due to the growth of dermatophytes, a type of fungus that thrives in warm, moist environments like locker rooms, showers, and even sweaty shoes. Symptoms include itching, burning, and stinging sensations, in addition to red, scaly, and cracked skin. Sometimes, it can also cause blisters or ulcers. Athletes and individuals who frequently wear tight-fitting shoes or who have sweaty feet are at higher risk. Diagnosis is typically made through a physical examination, and sometimes a skin scraping to confirm the presence of the fungus. Possible relief can include antifungal creams, powders, or sprays, and in more severe cases, oral medications. To prevent athlete’s foot, keep feet clean and dry, change socks regularly, wear breathable footwear, and avoid walking barefoot in communal areas. If you have athlete’s foot with persistent or severe symptoms, it is suggested that you visit a podiatrist for advanced treatment which often includes prescribed medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.
Types of Ankle Fractures

Ankle injuries can range from minor sprains to severe fractures. Broken ankles, or fractures, typically involve one or more of the three bones that make up the ankle joint. Specifically, they are the tibia and fibula in the leg, and the talus in the foot. The most common types of ankle fractures are lateral malleolus fractures, which affect the fibula. Medial malleolus fractures affect the tibia and bimalleolar fractures involve both the leg bones. Fractures that result in joint instability, may require surgery to ensure proper healing and reduce the risk of long-term complications, like arthritis. Rarer types of ankle fractures, such as trimalleolar fractures, Maisonneuve, or spiral, fractures, and talus fractures present their own unique challenges and treatment approaches. Symptoms of a fractured ankle include pain to touch, swelling, bruising and an inability to bear weight. If you have sustained a broken ankle, it is suggested that you make an emergency appointment with a podiatrist for a diagnosis and the appropriate treatment recommendations.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Cracked Heels and How to Prevent Them

Cracked heels, also known as heel fissures, are characterized by dry, thickened skin on the heels that splits or cracks. This condition often occurs due to factors such as dry weather, excessive standing or walking, improper footwear, or lack of proper foot care. When the skin becomes dry and loses its elasticity, it can crack under pressure, leading to painful fissures that may bleed or become infected, if left untreated. Prevention of cracked heels involves regular moisturizing to keep the skin hydrated and supple. Use a thick, emollient foot cream or lotion containing ingredients like urea or glycerin to help soften and moisturize dry skin. Exfoliating the heels regularly with a pumice stone or foot file can help remove dead skin cells and prevent the buildup of calluses. Additionally, wearing properly fitting shoes with adequate support and cushioning can reduce pressure on the heels and minimize the risk of developing cracked heels. If you have developed cracked heels that persist or become infected, it is strongly suggested that you visit a podiatrist for treatment.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Infection From Diabetic Foot Ulcers
 Foot infections from diabetes often stem from foot ulcers, open sores that develop due to poor circulation, and nerve damage linked to diabetes. If not properly managed, these ulcers can become infected and lead to serious health risks. Prevention is vital and involves maintaining stable blood sugar levels to enhance circulation and nerve function. Regular foot inspections are needed to catch ulcer formation early. Prevention strategies include daily foot cleaning and careful observation to identify changes before they worsen. Wearing appropriate footwear that reduces pressure points can also help prevent ulcers. Podiatrists, or foot doctors, also play an important role in diabetic foot care. These doctors can conduct regular check-ups to detect potential problems, recommend diabetic shoes, and teach proper foot care techniques. They will ensure that any foot concerns are addressed promptly. If you are at risk for diabetic foot ulcers or suspect a foot ulcer, it is suggested that you schedule an appointment with a podiatrist today.
Foot infections from diabetes often stem from foot ulcers, open sores that develop due to poor circulation, and nerve damage linked to diabetes. If not properly managed, these ulcers can become infected and lead to serious health risks. Prevention is vital and involves maintaining stable blood sugar levels to enhance circulation and nerve function. Regular foot inspections are needed to catch ulcer formation early. Prevention strategies include daily foot cleaning and careful observation to identify changes before they worsen. Wearing appropriate footwear that reduces pressure points can also help prevent ulcers. Podiatrists, or foot doctors, also play an important role in diabetic foot care. These doctors can conduct regular check-ups to detect potential problems, recommend diabetic shoes, and teach proper foot care techniques. They will ensure that any foot concerns are addressed promptly. If you are at risk for diabetic foot ulcers or suspect a foot ulcer, it is suggested that you schedule an appointment with a podiatrist today.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Podiatry Associates of Texas. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Arlington Weatherford, Mineral Wells, and Farmers Branch, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.